
Despite the availability of a wide range of antifungal agents, the incidence of invasive fungal infections and the resultant morbidity and mortality is on the rise in India. Along with the country’s warm, humid climate and a dusty atmosphere that are ideal for the growth of a variety of fungi, higher antifungal resistance and an increase in the number of immune-compromised hosts are the main reasons for growing affliction of these infections.
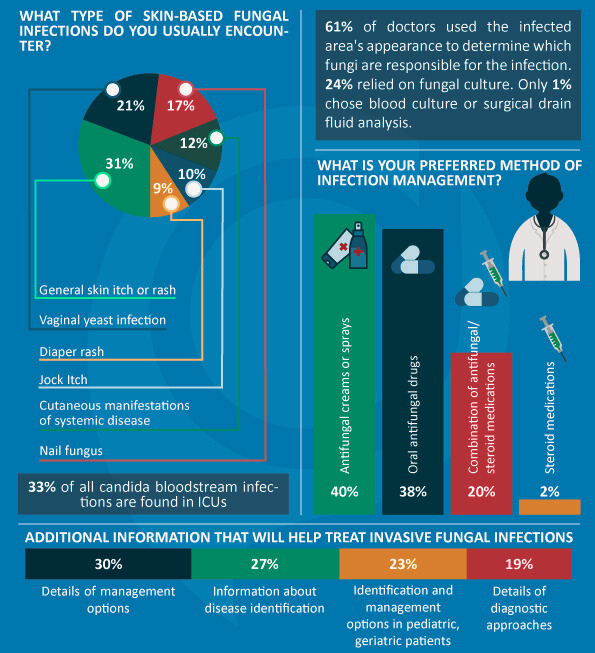
33% candida bloodstream infections occur in ICUs. This may be attributed to the higher use of a broad spectrum of antibiotics, prolonged survival on intensive care and increasingly complex procedures like organ transplantations, among other things. A major barrier to treatment is the lack of good diagnostic mycology laboratories and poor awareness amongst clinicians regarding the latest trends in diagnosis and management of fungal disease.
Focussed efforts by pharma to battle the emerging pathogens and educate doctors on various management options could decrease the morbidity, mortality and costs associated with fungal infections.
Docplexus’ latest survey reveals doctors’ opinions on managing invasive fungal infections in India.
Survey Details
Aim – To understand the various aspects related to diagnosis and treatment of invasive fungal infections amongst Indians.
Survey Methodology – Pan-India online poll on Docplexus members.
Sample Size – The survey was administered on 205 physicians out of which 150 completed it. General medicine practitioners and dermatologists comprised a majority of the respondents.
Survey Results
The survey revealed the following main trends:
- A majority of the skin-based fungal infections are itches or rashes – Diaper rash and jock itch were the least prevalent types of skin-based fungal infections in India. Skin itch/rash and nail fungus together accounted for 52% of all infections.
- The appearance of infected area is considered to be the best way to identify the fungi responsible for the infection – Over 60% of doctors rely on external examination of the infected area to determine fungi type. This reiterates their inclination toward limiting the use of diagnostic tests. This may partly be attributed to the fact that a majority of Indians cannot bear the burden of high medical costs, with less than 20% having medical insurance coverage. Blood culture and surgical drain fluid analysis are the least preferred modes for determining the fungi type. One disadvantage of blood culture is that it gives negative results in about 50% of cases of deep-seated candidiasis or gives positive results only late in the infection.
- Oral antifungal drugs and antifungal sprays or creams are the chosen methods of infection management – Since 78% of the doctors preferred to treat infections with antifungal agents rather than steroids, there is a need for more safe and effective antifungal medications. While lipid-based formulations of amphotericin B have lowered the risk of nephrotoxicity as compared to amphotericin B deoxycholate, they bear higher acquisition costs. Despite advances like echinocandins and newer triazoles, the failure in treatment and related mortality is quite high.
- Doctors need additional information for treating fungal infections – Doctors have unmet information needs in various aspects of the invasive fungal infections. 27% are on the lookout for information that helps to identify the disease. A majority of doctors feel that detailed information on the various options for managing the infection will result in better treatment. A significant number (23%) also seeks information specific to the pediatric and geriatric patient groups.
Older patients are more susceptible to invasive fungal infections owing to the higher likelihood of being treated with chemotherapy or immunosuppressive drugs for nonmalignant diseases. Certain aspects of histoplasmosis, aspergillosis and cryptococcosis are unique to geriatrics. Moreover, older patients are more likely to experience severe drug-drug interactions than younger ones. These factors pose different treatment challenges for doctors.
Pediatric patients differ from adults in terms of epidemiology, ways of diagnosis, pharmacokinetics and severity of adverse side effects of antifungal treatment. The various caregiving specialists (not necessarily pediatricians) need to be educated about these specifics so as to facilitate optimal treatment in this age-group.
Coming Up – Survey on Diagnosis and Management of Asthma
Past Surveys
Survey #4: Evaluating the Need for Awareness about Pediatric Vaccines
Survey #3: Assessing the Risks of Different Cardiovascular Diseases in India
Survey#2: Indian Doctors’ Opinions on Removal of Orthopedic Implants
Survey #1: What Doctors feel about Antibiotics Misuse
