Despite the availability of effective medical therapy for a long, Tuberculosis (TB) is one of the top five causes of death in India. In fact, the country is infamously termed, ‘the HUB of multi-drug-resistant (DR) TB’. Poor primary healthcare infrastructure in rural areas, un-monitored private healthcare, poverty, increasing affliction of diseases that compromise immune systems (e.g. HIV, diabetes, cancer), and rise in smoking and tobacco consumption are the main reasons of this huge disease burden.
The government has been grossly underestimating the incidence of TB for over 15 years, mainly due to the undercounting of TB cases in the private sector. Having only recently recognized the real scale of the disease burden (2.8 million new TB cases in 2015), the health ministry has begun work on a new National Strategic Plan to completely eradicate TB by 2025.
The success of this mission depends to a large extent on combined efforts of the medical community (notably general practitioners, consulting physicians and pulmonologists) and pharma companies.
Doctors’ Role
- Notify all TB cases to health authorities
- General Practitioners should understand classic TB symptoms to ensure fast diagnosis and immediate treatment
- Select the best drug regimen, based on DST (drug susceptibility testing)
- Play a supportive role to ensure patient compliance
Drug Manufacturers’ Role
- Ensure adequate supply of TB medicines
- Introduce more affordable drugs
- Improve bioavailability of drugs and reduce side effects
- Focus on FDCs (fixed-dose combinations) to reduce irregular intake or untimely discontinuation
Docplexus’ latest survey on physicians reveals the prevalent practices with respect to diagnosis and treatment of TB in India. It forms a part of a series to bridge the communication gap between doctors and pharma/medical device/diagnostic companies.
Survey Details
Aim – To assess doctors’ strategies for managing TB in India.
Survey Methodology – A pan-India online poll on Docplexus.
Sample Size – The survey was completed by 175 physicians. A majority were pulmonary/respiratory disease specialists or community medicine practitioners.
Survey Results
Key Insights
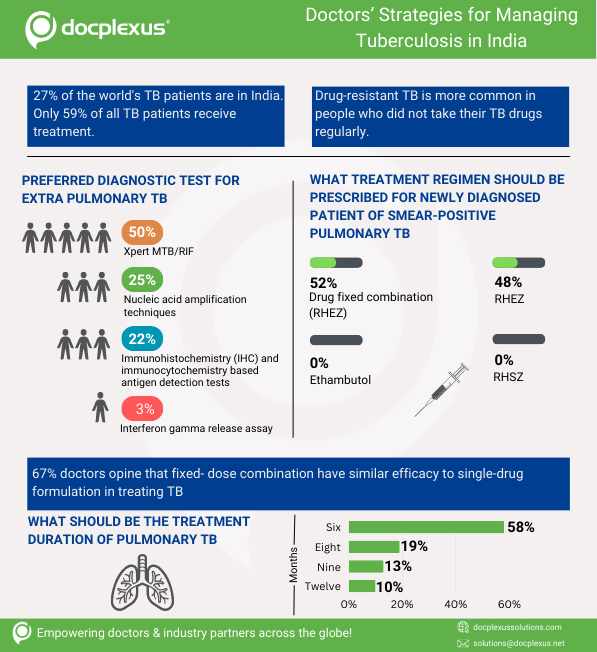
- Over half of all physicians vouch for Xpert MTB/RIF as the most reliable test to determine extra pulmonary TB – Extra pulmonary TB primarily affects the lymph nodes, meninges, kidney, spine, and growing ends of the bones. The main challenge in diagnosing this type is the frequently atypical clinical presentation that simulates other inflammatory and neoplastic conditions, leading to delay or deprivation of treatment.
Interferon Gamma Release Assay (IGRA) got the least votes as it cannot differentiate latent tuberculosis infection from tuberculosis disease. Also, it is a very expensive test. Nucleic acid amplification techniques are overly complex and cannot be used in most resource-limited settings. Therefore, only one-fourth of all doctors prefer these tests.
Xpert MTB/RIF can detect with high specificity a majority of extra pulmonary TB cases and is a useful rule-in test, especially while testing cerebrospinal fluid and tissue samples. It can be performed by clinicians with little training. This test is best suited for the requirements of the Indian healthcare setting.
- 56% of respondents claimed that irregularity in taking TB drugs is the largest cause of drug-resistant (DR) TB – DR TB is a human-made disease attributed to missed doses or halting the treatment mid-way. Although fully preventable, it often causes untold misery, suffering and economic loss. While Multi-DR TB is non-responsive to isoniazid and rifampicin, Extensively-DR TB is further resistant to fluoroquinolone (injectable). Totally-DR TB is not treatable.
India is estimated to witness a 152% increase in Multi-DR TB cases by 2032, 85% of which will be due to primary resistance. Only 19% of those with DR TB get proper treatment. However, the treatment is grueling with high toxicity of drugs, prolonged duration (2 years comprising 6 months of daily injections) and only a 50% chance of full recovery.
Additionally, most current medicines for treating Extensively-DR TB are very expensive and not readily available. It has been observed that over 40% of TB patients do not take the treatment regularly. It is vital for drug manufacturers to invest in the discovery of more effective, less toxic, and cheaper treatment options for TB. It is also important to educate doctors about the correct dosage and the ideal treatment duration.
- Most doctors opt for RHEZ to treat a newly-diagnosed patient of smear-positive pulmonary TB, fixed drug combination RHEZ scores slightly better than single-dose RHEZ – RHEZ (rifampicin, isoniazid, ethambutol and pyrazinamide) either in single-dose or fixed combination rapidly reduces the bacterial load. The most potent drugs, rifampicin and isoniazid, are continued after the intensive phase of first two months. No doctor chose ethambutol as a monotherapy. RHSZ (rifampicin, isoniazid, streptomycin and pyrazinamide) also did not find any takers. Although streptomycin was the first antibiotic known to control TB, currently, it is administered when primary resistance to others drugs is suspected.
- Fixed-dose combinations are perceived to have the same efficacy as single-dose formulations – Over two-thirds of all doctors find no difference in the efficacy of fixed-dose combinations (FDCs) and single-dose formulations. The WHO recommends FDCs as an additional step in the proper treatment of TB. FDCs’ advantages include simplified prescriptions, better management of drug supply and reduced risk of DR TB due to wrong drug selection or monotherapy. With FDCs, the number of tablets to be taken are reduced from 9-16 per day to only 3-4 during the entire course of treatment, improving patient compliance and reducing prescription errors.
However, it is essential that they have proven quality and rifampicin bioavailability. In most cases, poor drug quality rather than poor absorption is the main reason for inadequate blood levels of FDCs. Also, FDCs may be more expensive than the total cost of an individual single-drug tablet. It is important to note that no matter which approach is chosen (single-dose or FDC), DOTS (Directly Observed Therapy Short Term) cannot be done away with.
- 58% of doctors feel that 6 months is an adequate period for treating pulmonary TB – The length of TB treatment is determined by a number of factors such as the form of TB (active or latent), possible drug resistance, patient’s age and overall health. Multi-DR TB or extra pulmonary TB needs to be treated for longer durations. Similarly, the presence of diabetes mellitus and lung cavities at the start of treatment needs a prolonged continuation phase of treatment.
- About 10% of doctors feel that it takes one year to eradicate pulmonary TB. A majority (58%) however, opt for shorter durations – Recent research suggests that shorter terms treatment coupled with combined medication may be more effective as it may ensure better compliance and lower the risk of side effects. It is extremely essential to arrive at a consensus regarding the optimum treatment duration as prolonged or less than required intake of drugs may increase the risk of resistance.
Next Survey – Managing Osteoporosis
Past Surveys
Survey #6: Indian Doctors’ Opinions on Diagnosis and Management of Asthma
Survey #5: Management of Invasive Fungal Infections in India
Survey #4: Evaluating the Need for Awareness about Pediatric Vaccines
Survey #3: Assessing the Risks of Different Cardiovascular Diseases in India
Survey#2: Indian Doctors’ Opinions on Removal of Orthopedic Implants
Survey #1: What Doctors feel about Antibiotics Misuse
