
With healthcare is becoming more patient-centric, pharma is striving to design beyond the pill solutions that addresses patients’ pain points. It is believed that these offerings will not only lead to better treatment outcomes but also boost brand loyalty and advocacy by improving the overall experience.
Patient Support Programs (PSPs) are initiatives designed to add value to the patient community. PSPs aid physicians in medication therapy management. They redefine and broaden the concept of assistance, boost adherence to medication and consequently, improve effectiveness and quality of life for the patients.
While most early PSPs mainly addressed the issue of non-adherence, their scope has slowly expanded to include emotional well-being & lifestyle modifications. It is also expected that the focus will eventually shift from a mass-market approach to more customized offerings.
Since physicians play a role in recommending the right PSP to their patients, it is important to know their take on the strengths and drawbacks of existing support programs. Our community survey on PSPs in India revealed the following major opinions –
Survey Details:
Aim: To understand doctors’ viewpoint on patient support programs in India
Survey methodology: A nationwide online poll on Docplexus members
Sample size: 1,520 physicians comprising general physicians, community medicine practitioners, consulting physicians, family practitioners, psychiatrists & oncologists.
Survey Findings:
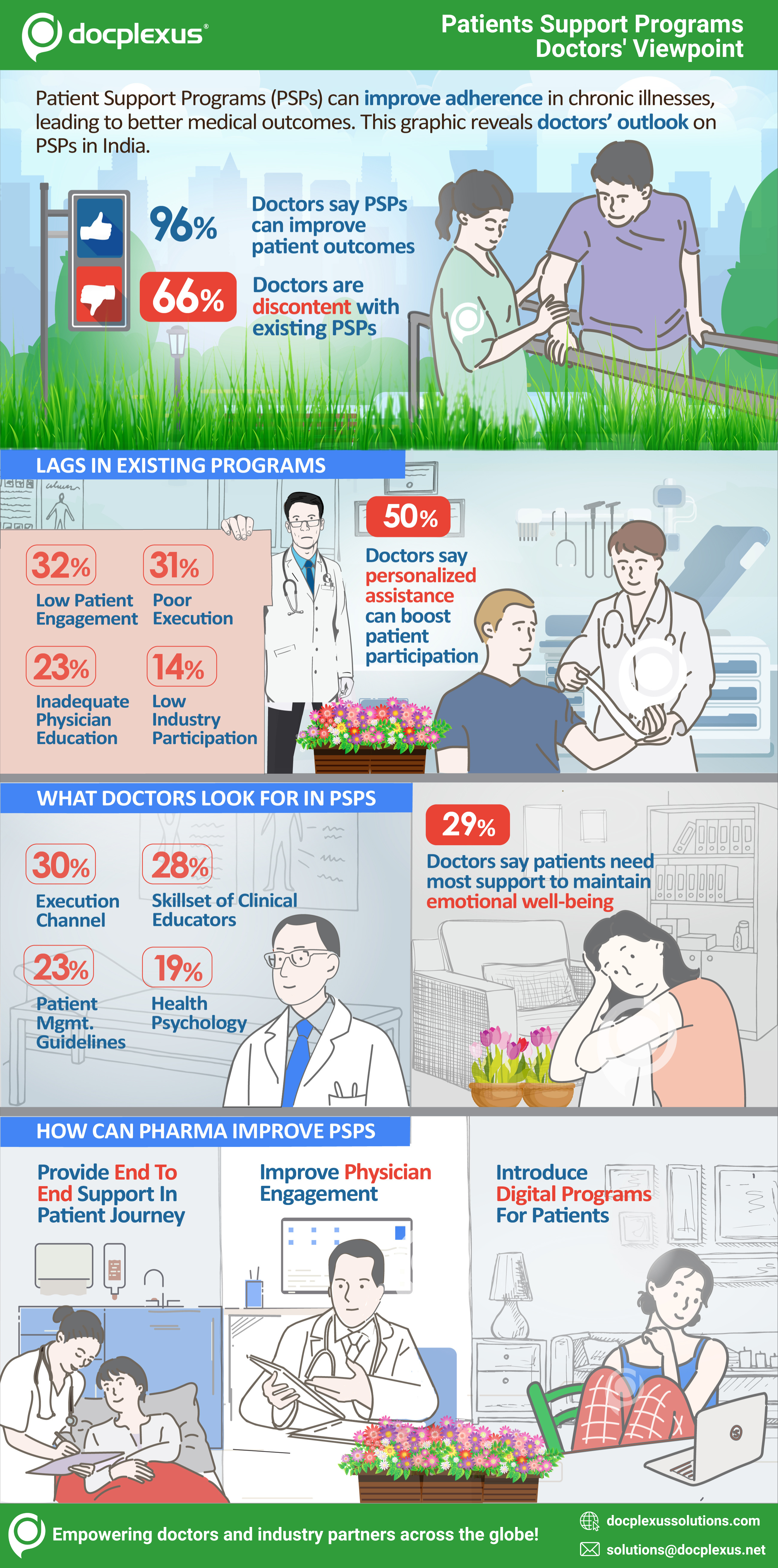
The survey revealed the following main opinions about PSPs –
Existing programs fail to deliver:
When the physicians were asked about the need for PSPs, almost all agreed that PSPs are an ideal way to directly support patients and help them achieve better medical outcomes. However, only 34% said that existing support programs are fulfilling the said objective of assistance and improved quality of life and 66% stressed the need for further improvements.
Loopholes in existing programs:
The majority of doctors, around 30%, felt that proper execution of the support programs and engagement with the patients was somewhere missing. Patients’ needs must be addressed and accordingly, the support programs need to be executed. One-on-one patient interaction and personalized assistance can help in improving patient adherence to these programs.
Considering the overall scenario of healthcare in India, it is observed that better participation from the industry will make a huge difference. More pharma firms need to come forward to initiate and execute these programs smoothly.
Another issue that needs to be addressed is the inadequate focus on helping patients, initiating treatment and overcoming the access challenges. Once the patient is diagnosed with a certain condition, it’s important that the support program caters to his journey from initiation of therapy to its conclusion. Every patient stage, right from the initial period (disease awareness, pre-prescription phase and initiation of therapy), to the latter part (access to medication, regular treatment follow-up and adherence), needs to be covered.
Another major problem is less than optimal involvement of the medical community. Many physicians, almost 23%, said that they needed better information and education about these initiatives so they fully understand the programs and help optimize their outcomes.
Need to focus more on emotional and social well-being:
Certain disorders like cancer or epilepsy have a huge impact on the patient’s life and family. Changes in the body can affect one’s self-esteem, confidence and arouse feelings of depression, anxiety, and suicidal tendencies. Support programs can help patients deal with such scenarios. A majority (29%) of doctors opined that emotional well-being is where patients need the most support.
Lifestyle modification is another area where doctors feel that patients need assistance. Disorders like Type 1 diabetes, metabolic syndrome, cancer, epilepsy or simply the prevention of Type 2 diabetes require that patients initiate lifestyle changes so as to reach their therapeutic goals. Around 21% of physicians stated that lifestyle modification strategies that target changes in behavior, physical activity, nutrition, etc., are important inclusions in the support programs. Few other aspects requiring support were medication directions (19%) and financial assistance (17%).
Thus, pharma companies must strive to determine the pain points of patients while designing PSPs.
Factors considered while recommending a PSP:
The survey results revealed that the skill level of clinical educators and an effective channel for execution were of prime importance to physicians while recommending the program to their patients. Further, patient management guidelines, health psychology plans, communication, and patient follow-up were some important factors considered.
How can Pharma improve PSP outcomes?
Physicians feel that pharma must play a more active role while carrying out support programs. They should think of innovative ways to improve patient participation and onboard doctors through digital awareness campaigns.
50% of respondents emphasized the need to offer personalized assistance via PSPs. With increasing comorbidities and specific conditions, PSPs will have to be more personalized. Such individualized support and intervention will help improve patient adherence and health outcomes. Pharma must find ways for patients to better manage medication, understand their condition and monitor their progress over time.
31% of respondents felt that Pharma should do a better job of involving physicians in these support programs. Giving them timely updates about the programs, sharing the patient progress, briefing about the patient guidelines used, having a timely report showing patient participation can help physicians remain updated about these support programs.
Fully tailored digital health support programs and awareness campaigns can take disease management to the next level. A digitally empowered patient community can actively manage medical conditions. Peer-to-peer and patient-physician conversations can be enabled to help patients in taking better control of their lives. Patients can share their experiences and support each other timely through digital connect. Including appropriate tools, data captures, alerts and progress tracking can further improve program outcomes. Digital therapeutics could play a key role in PSPs in the future. It is expected that next-gen patient support would use behavioral science and real-world data and this will lead to a paradigm shift in patient outcomes.
A more holistic approach will help Pharma realize the true potential of PSPs. This, combined with the right digital support can prove to be a game-changer in improving healthcare outcomes.
What Are Your Suggestions to Improve Patient Support Programs?
Docplexus – Pharma’s Trusted Marketing Partner
Docplexus is one of the world’s largest & fastest-growing networks of verified doctors & a trusted marketing partner of pharma, medical devices, diagnostics & nutraceutical companies. We empower our industry partners to meaningfully engage with the medical community through data-driven, evidence-based marketing & brand management solutions such as infocenter (branded microsite), mindset analysis, KOL webinars, sponsored medical updates, online CMEs & more.
